Does lack of sleep harm your organization?
The impact
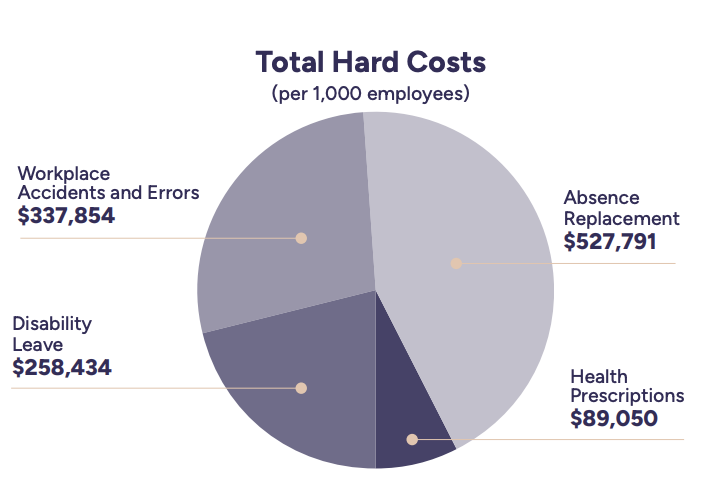
There are 5 significant sleep-related business costs that are hurting your organization.
Let’s review each of them under the assumption
that your employees earn an average salary of
$80,000 per year.1
1. Increased productivity losses
Employees with poor sleep will miss work up to 3 times more often than good sleepers and have their productivity negatively impacted up to 46 days per year.1

Over half of us (51%) suffer from poor sleep to some degree3, including the 19%2 of the general population that experience chronic insomnia. In professions with non-daytime schedules or rotating shifts, the chronic insomnia rate can be twice as high. No matter your organization, sleep-related issues are creating a real but often invisible productivity burden.
2. More frequent and higher disability leave costs
Poor sleepers are 4.6 times more likely to go on disability leave than good sleepers.4 With that in mind, it’s no wonder that 33% of all claimants experience chronic insomnia at the time they go on disability.4

Poor sleep has been shown by repeated studies to be strongly associated with mental health issues, including anxiety and depression.4
3. Increased absence-replacement costs
High rates of sleep-related absenteeism and disability leave also drive higher replacement costs for roles that require replacement workers when an employee doesn’t show up.

4. More frequent and costly workplace accidents and errors
Poor sleep is responsible for nearly 25% of the total cost of all workplace accidents and errors.6 Being awake for 17 hours is similar to having a blood alcohol concentration (BAC) of 0.05%, while being awake for 24 hours is similar to having a BAC of 0.10%(above the legal limit of 0.08%).7

Poor sleep drives a range of symptoms that have an insidious effect on safety, including difficulty concentrating and focusing as well as poor decision-making.
5. Prescription medication costs
On average, roughly 10% of workers depend on prescription medication to sleep.8 In professions with non-daytime schedules or rotating shifts the prescription medication rate for sleep can be significantly higher.9

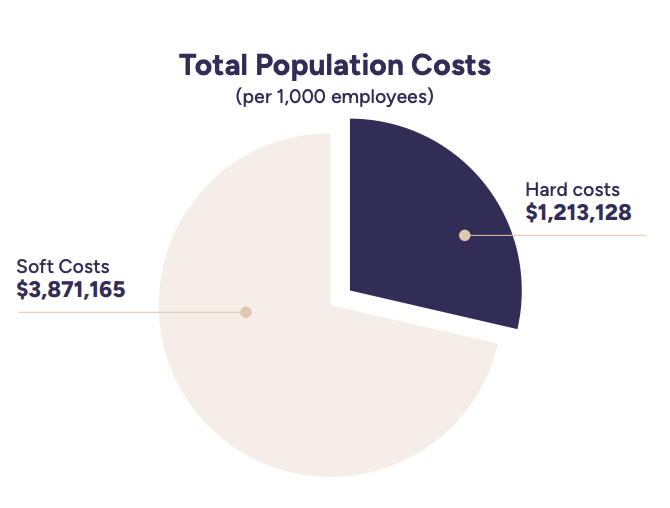
The cost of lack of sleep for the entire working population
The HALEO Solution
Best-in-class clinical outcomes:
- Over 85%* of HALEO patients complete their treatment, compared to less than 50% with internet-based cognitive behavioural therapy (iCBT) and other self-guided solutions in real-world settings,10 and around 70%11 with traditional therapist-led interventions in the community.
- Patients give HALEO a 90%* satisfaction score.
- 94%* of HALEO patients no longer show clinically significant symptoms post-treatment, typically within 5 weeks.
Our proprietary and exclusive Cognitive Behavioural Therapy for Insomnia (CBT-I) approach is proven and clinically validated. Thanks to its brief, engaging session format, the duration and burden of treatment are significantly reduced compared to a traditional, group therapy-based clinical setting.
HALEO is designed to save employers money by keeping their people at work, with fewer injuries, fewer errors, and more focus.
An investment
When we implement HALEO within an organization, we work with our customers to ensure a high rate of employee engagement.
of their workforce is engaged
Through clear communication and education for employees on the benefits and importance of good sleep, many HALEO customers are able to engage more than 25%.

ROI gain
Many HALEO customers’ achieve a return on investment of over 10 times the cost of the solution.
Improved sleep leads
to improved mental health
References
2 Morin, C. M., Vézina-Im, L. A., Ivers, H., Micoulaud-Franchi, J. A., Philip, P., Lamy, M., Savard, J. (janv. 2022). «Prevalent, incident, and persistent insomnia in a population-based cohort tested before (2018) and during the first-wave of COVID-19 pandemic (2020)», Sleep, 45(1):zsab258. doi : 10.1093/sleep/
zsab258. PMID : 34698868; PMCID : PMC8574325.
6 Shahly, V., Berglund, P. A., Coulouvrat, C., Fitzgerald, T., Hajak, G., Roth, T., Shillington, A. C., Stephenson, J. J., Walsh, J. K., Kessler, R. C. (oct. 2012). «The associations of insomnia with costly workplace accidents and errors: results from the America Insomnia Survey», Archives of General Psychiatry,
69(10):1054-1063. doi : 10.1001/ archgenpsychiatry.2011.2188. PMID : 23026955.
7 Arnedt, J. T., Owens, J., Crouch, M., Stahl, J., Carskadon, M. A. (2005). « Neurobehavioral performance of residents after heavy night call vs after alcohol ingestion », JAMA, 294:1025-1033. Dawson, D. et Reid, K. (1997). «Fatigue, alcohol and performance impairment», Nature, 388:235. Williamson, A. M. et Feyer, A. M. (2000). « Moderate sleep deprivation produces impairments in cognitive and motor performance equivalent
to legally prescribed levels of alcohol intoxication », Occupational and Environmental Medicine, 57:649-655.
8 National Center for Health Statistics (2020). National Health Interview Survey.
9 Tucker, P., Härmä, M., Ojajärvi, A., Kivimäki, M., Leineweber, C., Oksanen, T., Salo, P., Vahtera, J. (déc. 2021). « Association of rotating shift work schedules and the use of prescribed sleep medication: A prospective cohort study », Journal of Sleep Research, 30(6):e13349. doi : 10.1111/jsr.13349. Epub 14 juin 2021. PMID : 34128266.
10 L’étude porte sur la TCC en face à face (et non sur l’insomnie) et nous avons
un taux d’achèvement de 85 % (Fernandez et coll., 2015). Ritterband, L. M., Thorndike, F. P., Morin, C. M., Gerwien, R., Enman, N. M., Xiong, R., Luderer, H. F., Edington, S., Braun, S., Maricich, Y.A. (juin 2022). «Real-world evidence from users of a behavioral digital therapeutic for chronic insomnia», Behaviour Research and Therapy, 153:104084. doi : 10.1016/j.brat.2022.104084. Epub 1er avril 2022. PMID : 35405424.
11 Ong, J. C., Kuo, T. F., Manber, R. (avr. 2008). « Who is at risk for dropout from group cognitive- behavior therapy for insomnia? », Journal of Psychosomatic Research, 64(4):419-425. doi : 10.1016/j.jpsychores.2007.10.009. PMID : 18374742; PMCID: PMC2435302.

